What is Atrial Fibrillation?
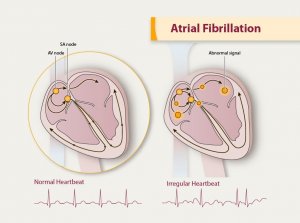
Image Source: Google
Atrial Fibrillation, also referred to as AFIB, is a common health condition that causes your heart to beat abnormally. The electrical impulses in your heart do not transmit across the heart muscle correctly, causing your heart rhythm to be irregular and too fast. AFIB is often described as a flutter or quivering heartbeat. AFIB may cause symptoms such as shortness of breath, chest pain, heart palpitations, and fatigue, but some people may not experience any symptoms. An irregular heartbeat means your heart is not pumping blood properly which can lead to a significant increase in the risk of blood clots and stroke (CDC.gov, 2020).
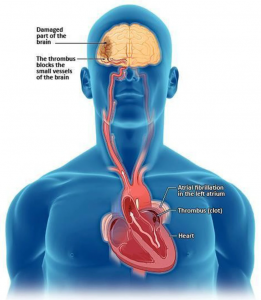
Image Source: Google
Is Atrial Fibrillation Preventable?
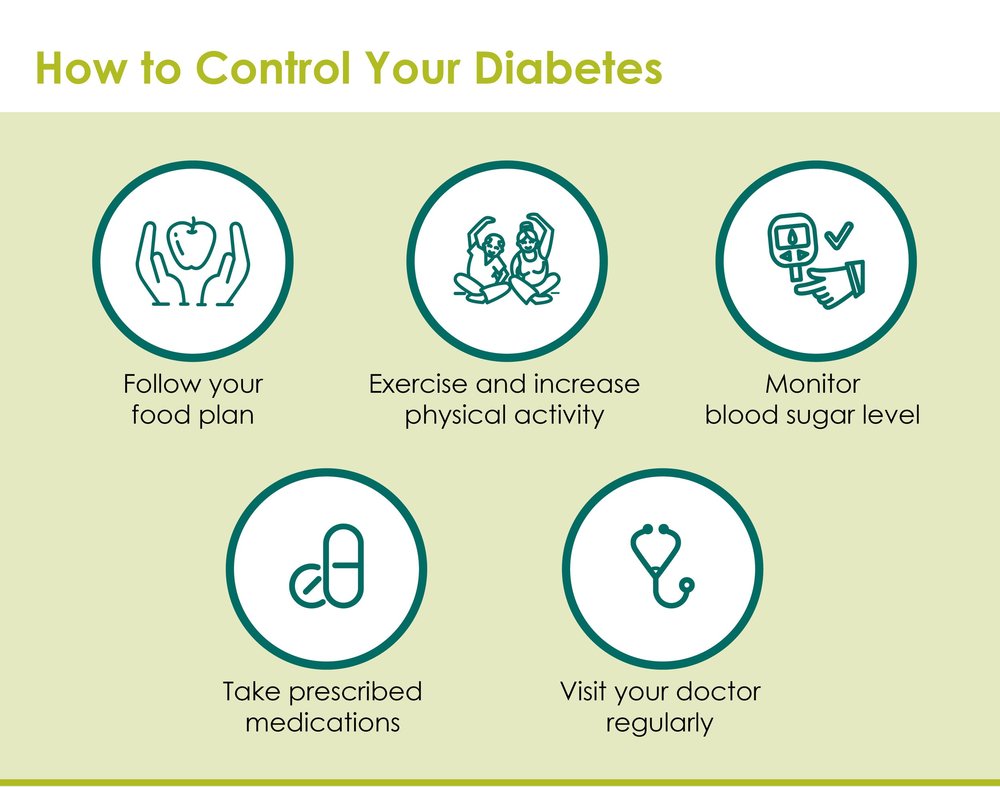
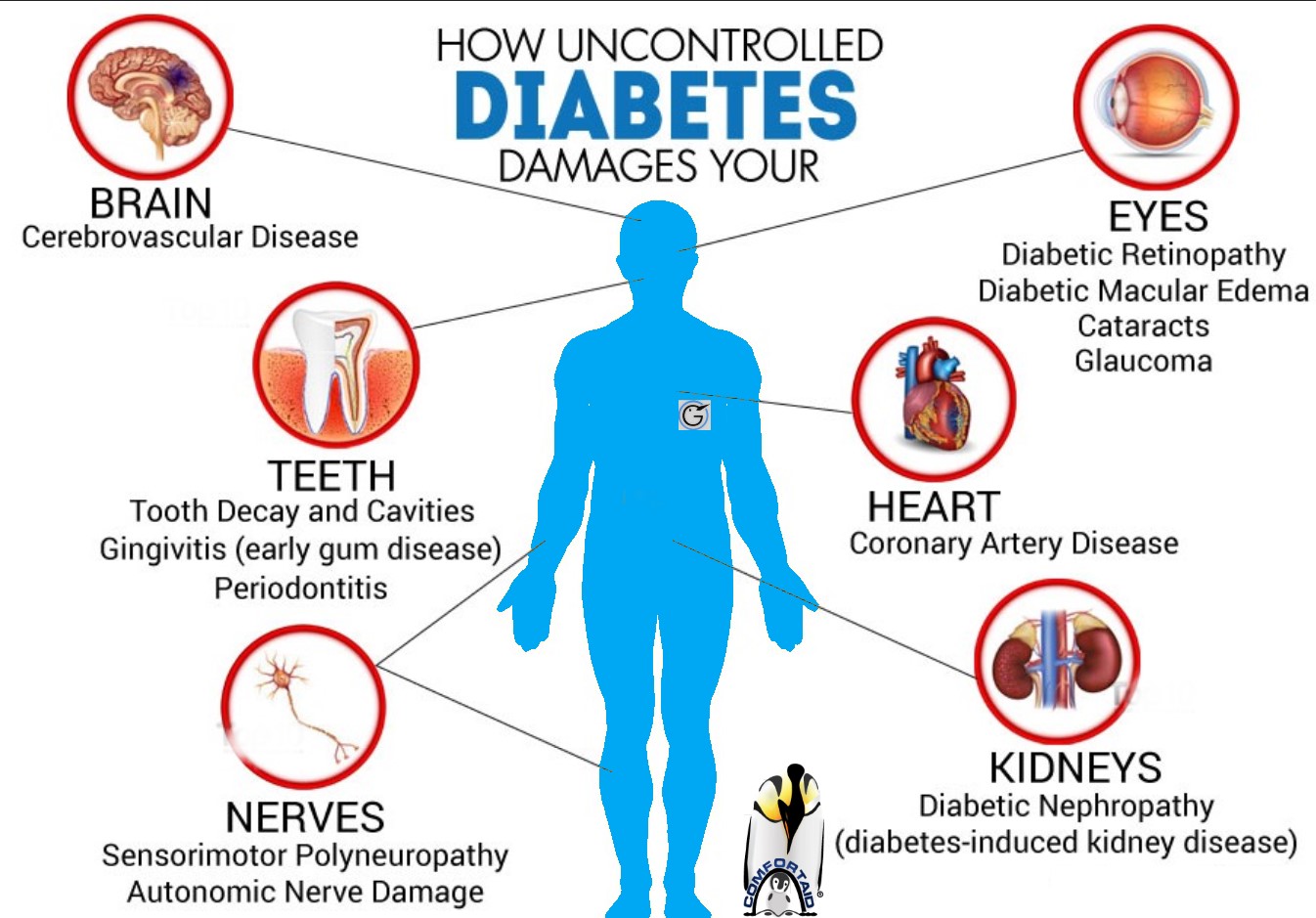
There are two aspects to the risk of developing AFIB, genetic factors, and lifestyle factors. Genetic factors cannot be modified but making lifestyle changes can decrease the risk of developing AFIB. Recent research indicates that several common risk factors related to the development of AFIB are related to lifestyle choices and therefore reversible with behavioral changes. The major risk factors for AFIB are obesity, physical inactivity, sleep apnea, diabetes mellitus, hypertension, and alcohol and tobacco use. By visiting your doctors regularly, losing weight, stopping smoking and drinking alcohol, exercising, and eating a healthy diet, most risk factors are modifiable and can lead to lower chances of developing AFIB and precursors of AFIB (Chung et al., 2020).
Can eating chocolate reduce your risk of AFIB?
Video Link: Chocolate linked to lower risk for heart condition
Claims have been made that consuming a certain amount of chocolate regularly can lower your risk for developing AFIB, however research studies have found contradictory results. Because chocolate contains substances thought to be beneficial for cardiovascular health, it may help prevent other conditions but there is still debate among the medical community in regards to AFIB (Khawaja et al, 2015). You should consult your physician before adding chocolate to your diet for this purpose, especially if you have other health conditions, such as diabetes mellitus.
Can drinking alcohol increase your risk of AFIB?
Recent research studies have found strong associations between alcohol consumption and the development of AFIB. Evidence indicates that even small amounts of alcohol are related to an increased risk for AFIB. People at risk for AFIB should seriously consider reducing their daily alcohol consumption to one glass or less per day, or abstaining from drinking alcohol altogether (Csengeri et al., 2021).
Can Atrial Fibrillation be diagnosed by your smart watch?
Video Link: Smart watches are making more people aware of their heartbeats and irregular heartbeats
Recent news reports have made the claim that smart watches with the ability to monitor heart rate and record an electrocardiogram may be able to diagnose AFIB. While studies have found that smart watches may be potentially useful, at the present time the technology still has too many issues and inconsistencies to be considered appropriate for the diagnosis of heart rhythm problems. Smart watches should never be used as an alternative to visiting your doctor and undergoing formal diagnostic testing.
References
CBS News. (2017, May 24). Chocolate is linked to lower risk for heart condition AFib. CBS News. https://www.cbsnews.com/news/chocolate-linked-to-lower-risk-for-atrial-fibrillation-heart-health
Centers for Disease Control and Prevention. (2020, September 8). Atrial Fibrillation. cdc.gov. https://www.cdc.gov/heartdisease/atrial_fibrillation.htm
Chung, M. K., Eckhardt, L. L., Chen, L. Y., Ahmed, H. M., Gopinathannair, R., Joglar, J.A., Noseworthy, P. A., Pack, Q. R., Sanders, P., & Trulock, K. M. (2020). Lifestyle and Risk Factor Modification for Reduction of Atrial Fibrillation: A Scientific Statement From the American Heart Association. Circulation, 141(16), e750–e772. https://doi.org/10.1161/CIR.0000000000000748
Csengeri, D., Sprünker, N.-A., Di Castelnuovo, A., Niiranen, T., Vishram-Nielsen, J. K., Costanzo, S., Söderberg, S., Jensen, S. M., Vartiainen, E., Donati, M. B., Magnussen, C., Camen, S., Gianfagna, F., Løchen, M.-L., Kee, F., Kontto, J., Mathiesen, E. B., Koenig, W., Stefan, B., & de Gaetano, G. (2021). Alcohol consumption, cardiac biomarkers, and risk of atrial fibrillation and adverse outcomes. European Heart Journal, 42(12), 1170–1177. https://doi.org/10.1093/eurheartj/ehaa953
Fox14now.com. (2021, Jul 14). Smart watches are making more people aware of their heartbeats and irregular heartbeats. Fox13now.com. https://www.fox13now.com/the-place/smart-watches-are-making-more-people-aware-of-their-heartbeats-and-irregular-heartbeats
Haverkamp, W., Butler, J., & Anker, S. D. (2021). Can we trust a smartwatch ECG? Potential and limitations. European Journal of Heart Failure, 23(6), 850–853. https://doi.org/10.1002/ejhf.2194
Khawaja, O., Petrone, A. B., Kanjwal, Y., Gaziano, J. M., & Djoussé, L. (2015). Chocolate Consumption and Risk of Atrial Fibrillation (from the Physicians’ Health Study). American Journal of Cardiology, 116(4),563–566. https://doi.org/10.1016/j.amjcard.2015.05.009
PatientEducation.Video. (2017, May 1). Alcohol and Atrial fibrillation, by Dr. Carlo Oller. Youtube.com. https://www.youtube.com/watch?v=JH8ekR2SI8M