Does consumption of Whole Grains reduce the risk of Heart Disease?
It is a common question that merits more than a one line answer. To evaluate and understand the advantages of consumption of Whole Grains in the prevention of Heart Disease, firstly, we needed to understand what is considered Heart Disease, what is the definition of Whole Grains and when is a diet considered to be whole-grain diet. There is a lot of information in the media and they sometimes seem to directly contradict each other.

© Copyright 2017 – Brooke Findley
What is Heart Disease?
The conditions commonly referred to as Heart Disease are known as Cardiovascular Diseases or CVD in medical terms. CVD are a group of conditions that affect the heart and blood vessels and include coronary heart disease, cerebrovascular disease, and peripheral arterial disease. Cardiovascular disease occurs when the arteries are completely blocked or when blood flow is restricted by a narrowed artery, limiting the amount of blood and oxygen delivered to organs or tissue. Cardiovascular disease is the number one cause of death and disability globally. Around 30% of total global deaths can be attributed to CVD, and it is estimated to cause 17 million deaths per year. The World Health Organization reports that by 2030, CVDs will account for almost 23.3 million deaths per year and could increase due to aging populations and increasing levels of sedentary lifestyles and obesity
What are Whole Grains?
Whole grains consist of the intact, ground, cracked or flaked kernel of the grain after the removal of inedible parts such as the hull and husk. Whole grain kernels contain all three parts: the bran, germ, and the starch. Refining grain removes the healthiest part, the bran and the germ, leaving only the starch. Whole grains are important sources of nutrients like zinc, magnesium, B vitamins, and fiber.
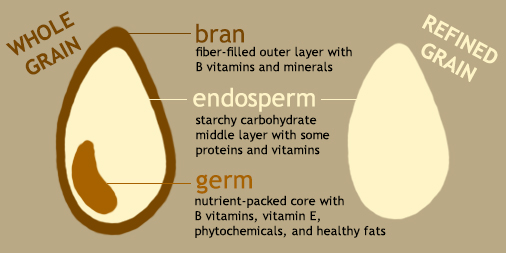
© Copyright 2014 – Harvard School of Public Health
Whole grains are grains that come from grasses such as wheat, oats, rice, corn, barley, sorghum, rye, and millet. Some non-grains that do not come from grasses but are cooked and consumed in a similar manner are also considered whole, such as quinoa, buckwheat, and amaranth.
How do I know food is rich in Whole Grains?
For foods made from whole grain such as breads, breakfast cereals, pasta, biscuits, and grain-based snack foods, a standard definition for what constitutes a whole grain food has been recommended as a minimum of 8 g whole grains/30 g serving or in other words, 27 g whole grains/100 g serving.
What is the benefit of Whole Grain consumption?
A whole grain contains the entire edible parts of a natural grain kernel and are excellent sources of dietary fiber while most refined grains contain little to no fiber. Dietary fiber from whole grains, as part of an overall healthy diet, help improve blood cholesterol levels, and lower risk of heart disease, stroke, obesity and type 2 diabetes
What are the common misinformation about Whole Grains?
- Refined Grains and Whole Grains are equally rich in nutritional values and fiber.
- Whole Grains are high is starch and should be avoided for people with Type 2 Diabetes.
- Consumption of Whole Grains will prevent Heart Attacks.
- Whole grains cannot be consumed by people who have gluten-free diet needs.
Let us answer some of these false narratives.
- Whole grains and Refined Grains do not have similar nutritional value or fiber
Whole grains contain all three parts of the kernel: the bran, germ, and endosperm. Whole grains are rich in dietary fiber, antioxidants, resistant starch, phytoestrogens, and other important micronutrients such as vitamins and folic acid. Refining normally removes most of the bran and some of the germ, resulting in the loss of dietary fiber, vitamins and minerals. Without the bran and germ, about 25% of a grain’s protein is lost, and grains are greatly reduced in at least seventeen key nutrients. After removal of bran and germ, the remaining starchy endosperm is ground to produce refined white flours.
- Whole Grains are richer in fiber than Refined Grains, thus good for people with Type 2 Diabetes
Whole grain much richer in fiber than refined grains and though whole grains contain starch, the percentage of starch is much greater in refined grains. Further, because of higher fiber, consumption of whole grains make a person feel fuller and that results in consumption of lesser carbohydrates. Studies have found that compared with those who rarely or never consume whole grains, those reporting an average of 48–80 grams/day of whole grain had a 26% reduction in Type 2 Diabetes risk and a 21% reduction in CVD risk factors.
- Whole Grain consumption does not prevent heart attacks
There are some studies that show definite benefits in consumption of whole grains and there are other studies which are somewhat skeptical. Even studies that do not support the direct benefit of whole grain show evidence of supplementary dietary improvements, such as increased consumption of dietary fiber, associated with the consumption of whole grains that are found to have benefits in the reduction of some of the risk factors associated with Type 2 Diabetes and Heart Disease. However, there are no studies that conclude that heart attacks can be prevented by consumption of Whole Grains.
- Can whole grains be gluten free?
The short answer is: Yes. There are many whole-grain products, such as buckwheat, gluten-free oats, popcorn, brown rice, wild rice, and quinoa that fit gluten-free diet needs.
How to add Whole Grains to my diet?
Now that we know that consumption of whole grains reduces the risk factors associated with Heart Disease and Type 2 Diabetes, you might want to know how to add more whole grains to your meals. To include more whole grains and boost the fiber content of meals, try making simple changes to your cooking habits. Partner whole grains — brown rice and vegetable stir-fry or a whole-wheat pita stuffed with salad. Fortify mixed dishes with high-fiber ingredients — try adding bran or oatmeal to meat loaf.
Looking for other ways to add whole grains?
- In breakfast: Choose a fiber-rich, whole-grain breakfast cereal, oatmeal or toast. Check the grams of fiber per serving; more fiber will keep you feeling fuller, longer.
- For Lunch: Choose whole grains over refined items when selecting breads, buns, tortillas, pastas, brown rice and other grains.
- For Dinner: Experiment cooking with grains such as buckwheat, bulgur, millet, quinoa, sorghum, whole rye or barley.
- As a snack: Three cups of whole-grain, air-popped popcorn contains 3.5 grams of fiber and only 95 calories. Try 100-percent whole-wheat or rye crackers.
How to find Whole Grains? While selecting food with whole grains, what to look for in Food Labels?
Remember, being brown doesn’t make bread whole wheat and being white may not mean that bread is made with just refined white flour. Finding whole-grain breads takes some label reading skills. Any bread labeled “whole wheat” must be made with 100-percent whole-wheat flour.
Also, did you know that even if bread labels advertise “seven-grain” or “multigrain,” they are not necessarily whole-grain products? Check the Nutrition Facts panel to make sure whole-wheat flour is listed as the first ingredient and find loaves made mostly with whole-wheat or other whole-grain flour.
These are just some ways to ensure whole grain consumption; there are many ways to add whole grains to your daily diet. For more information, visit the websites in the references below.
Remember, whole grains won’t do miracles but will surely contribute to a heart healthy diet!
References:
- American Heart Association
http://www.heart.org - Academy of Nutrition and Dietetics
https://www.eatright.org/food/nutrition/dietary-guidelines-and-myplate/how-to-add-whole-grains-to-your-diet - The 9 Essential Whole Grain Foods You Need in Your Diet
https://www.cookinglight.com/nutrition-101/essential-whole-grain-foods-you-need-your-diet - Health Department Missouri
http://butlercountyhealth.org/2013/09/03/10-tips-for-choosing-whole-grains/ - Whole grain cereals for the primary or secondary prevention of cardiovascular disease.
https://library.neit.edu:2404/10.1002/14651858.CD005051.pub3 - The Cochrane Database of Systematic Reviews, 8, CD005051. Disease, Heart Disease and Coronary Heart Disease, 2018.
https://www.nhlbi.nih.gov/sites.









:max_bytes(150000):strip_icc():format(webp)/nutrition-during-pregnancy-4172730-5bc3f60c46e0fb0026718692.png)







 Constant noise. Loud noises prevent sleep
Constant noise. Loud noises prevent sleep