By: Tyler Read
By: Tyler Read
What is Dialysis?
Healthy kidneys clean your blood, remove extra fluid from your body in the form of urine, and remove toxins from your blood. Dialysis is a form of treatment that replaces some of these functions when your kidneys no longer work. Starting dialysis comes with many life changes, including changes to your diet.
In this video created by the National Kidney Foundation, Belinda Jim MD speaks about the specific diet needs of dialysis patients. These include restricting the amount of fluid you consume, restricting the amount of potassium in your diet, and restricting the amount of phosphorus in your diet. In agreement with Belinda Jim MD, Estridge et al. (2018), recognizes that fluid restriction adherence can help you feel comfortable prior to, during, and after your hemodialysis treatments. Although dialysis treatments help remove excess fluid and waste in your body, it does not do it as effectively as healthy kidneys. Consuming more than your recommended fluid allowance can cause edema (swelling), hypertension (high blood pressure), and difficulty breathing from fluid building in your lungs (Estridge et al., 2018). A registered dietitian (RD) can help you with your individual fluid restriction needs.
DaVita dialysis is a leading provider in kidney care who provide services for patients with chronic kidney disease and end-stage renal failure. In this video, Jackie, a DaVita RD, provides tips on how to limit fluid intake throughout the day, since your kidneys can not remove excess fluid from your body. To successfully manage fluid restrictions, you must know how to appropriately measure your fluid intake (Parker, 2019). This tip from Jackie is just one way to ensure you are measuring your fluid intake.
Potassium:
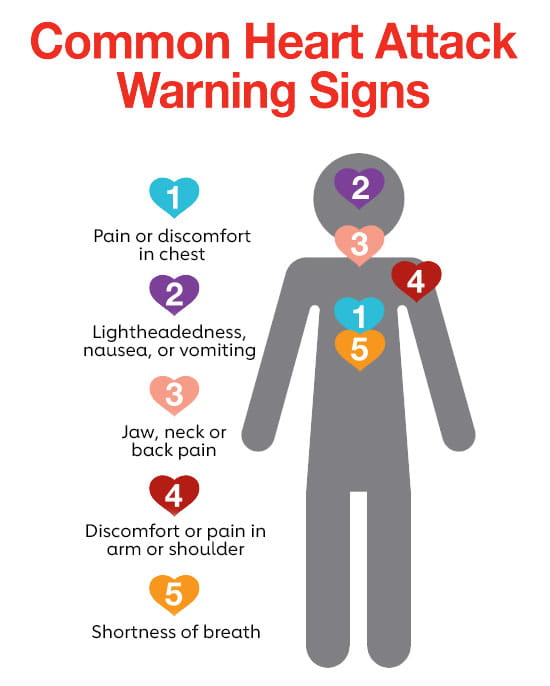
As Belinda Jim, MD mentioned in the first video, potassium restriction is an important part of the renal diet. The mineral, potassium, controls nerve and muscle function, and is found in many foods. Potassium helps your heart beat a normal rhythm and is necessary for electrolyte balance, pH balance, and maintaining fluid balance. Too much potassium can be dangerous. Normally functioning kidneys are able to remove extra potassium from your body, but in people with kidney disease, the potassium can build up and be dangerous. In agreement with Belinda Jim, MD, Anderson & Nguyen (2018), recommend that potassium intake be reduced. Your RD can help you figure out your specific potassium needs. Some foods to limit or avoid include (Parker, 2019):

By: Pedro Alonso

By: Mike Mozart

By: Stock Catalog

By: Rebecca Siegel
Phosphorus:
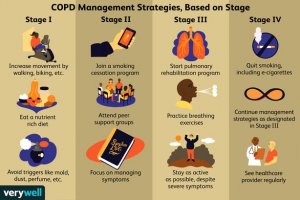
As Christy Turner, RD, from UC San Diego Chronic Kidney Disease Program mentioned in the video, phosphorus is a mineral that aids your body in keeping your bones healthy and helps keep your blood vessels and muscles strong. It is found in foods such as meats, poultry, fish, nuts, and beans. It can also be added to foods and used as a preservative. If your phosphorus becomes too high, you can experience itchy skin, weak bones, and bone and joint pain. High blood phosphorus can lead to an increased risk for bone disease (Anderson & Nguyen, 2018). If you have too high of phosphorus, your RD may recommend a diet restriction. Food to avoid or limit if your phosphorus is too high include (Anderson & Nguyen, 2018):

By: Mike Mozart

By: Paul Wilkinson

By: Rebecca Siegel
Hemodialysis patients often struggle with renal diet compliance due to how restricting the diet can be (Lederman, 2018). Restricting fluid, potassium, phosphorus, and adhering to treatments can be a daunting task for most patients (Lederman, 2018). There are many credible sources available online to help you navigate your renal diet needs. However, consulting with your RD about your individualized diet needs before looking up additional information is recommended.
References
Anderson, C. A. M., & Nguyen, H. A. (2018). Nutrition education in the care of patients with chronic kidney disease and end-stage renal disease. Seminars in Dialysis, 31(2), 115–121. https://doi.org/10.1111/sdi.12681
Estridge, K. M., Morris, D. L., Kolcaba, K., & Winkelman, C. (2018). Comfort and Fluid Retention in Adult Patients Receiving Hemodialysis. Nephrology Nursing Journal, 45(1), 25–60.
Lederman, A. (2018). Taking the Renal Diet on a Field Trip…2018 ANNA National Symposium, Las Vegas, NV. April 15-18, 2018. Nephrology Nursing Journal, 45(2), 200.
Parker, J.R. (2019). Use of an educational intervention to improve fluid restriction adherence in patients on hemodialysis. Nephrology Nursing Journal, 46(1), 43-47.