What is HPV?
HPV (Human Papilloma Virus) is the most common sexually transmitted infection. There are 79 million Americans, most in their late teens and early 20s, are infected with HPV. There are many different types of HPV. Some types can cause health problems including genital warts and cancers. There are vaccines that can stop these health problems from occurring.
How does HPV spread?
HPV by having vaginal, anal, or oral sex with someone who has the virus. It is most commonly spread during vaginal or anal sex. HPV can be passed even when an infected person has no signs or symptoms. Anyone who is sexually active can get HPV, even sexual activity with only one person. You can develop symptoms years after you have sex with someone who is infected. This makes it hard to know when you first became infected.
HPV & Cancer
HPV can cause cervical and other cancers including cancer of the vulva, vagina, penis, or anus. It can also cause cancer in the back of the throat, including the base of the tongue and tonsils. Cancer often takes years to develop after a person gets HPV. The types of HPV that can cause genital warts are not the same as the types of HPV that can cause cancers. The lag in time from infection to showing symptoms makes it hard to pinpoint the exact time of infection.

HPV Prevention
- Use Condoms
- Engage in monogamous relationships
- Get vaccinated
Who can get vaccinated?
HPV vaccination is recommended at age 11 or 12 years and for everyone through age 26 years, if not vaccinated already. Vaccination is not recommended for everyone older than age 26 years. Some adults age 27 through 45 years who are not already vaccinated may get the HPV vaccine after speaking with their healthcare provider about their risk for new HPV infections and the possible benefits of vaccination. HPV vaccination in this age range provides less benefit. Most sexually active adults have already been exposed to HPV, although not necessarily all of the HPV types targeted by vaccination.

Vaccine in vial with syringe. Vaccination concept. 3d









 There have been strides in recent years to prevent medication errors such as the report that was published “To Err is Human”, and the implementation of the five rights of medication administration.
There have been strides in recent years to prevent medication errors such as the report that was published “To Err is Human”, and the implementation of the five rights of medication administration.



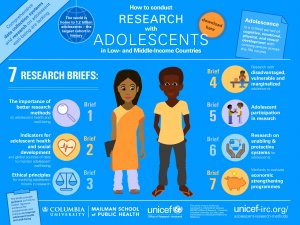 Physical changes from puberty can continue into middle adolescence. Most males at this point will begin their growth spurt, and puberty related changes will continue. Their voices may get deeper and acne may appear. At this point the physical changes may be nearly finished for females, and most typically have regular periods. Also at this age, many teens begin to explore romantic and sexual relationships. They may begin to question and explore their sexual identity. This can also be a stressful time if they do not have steady support from peers or family. Many middle adolescents have more arguments with their parents as they continue to struggle for independence. They may begin to spend more time with their peers compared to their families, causing peer pressure to peak at this age. The brain also continues to change and mature at this stage, but there still are many differences in how these middle adolescent think compared to adults.
Physical changes from puberty can continue into middle adolescence. Most males at this point will begin their growth spurt, and puberty related changes will continue. Their voices may get deeper and acne may appear. At this point the physical changes may be nearly finished for females, and most typically have regular periods. Also at this age, many teens begin to explore romantic and sexual relationships. They may begin to question and explore their sexual identity. This can also be a stressful time if they do not have steady support from peers or family. Many middle adolescents have more arguments with their parents as they continue to struggle for independence. They may begin to spend more time with their peers compared to their families, causing peer pressure to peak at this age. The brain also continues to change and mature at this stage, but there still are many differences in how these middle adolescent think compared to adults.
 check their blood sugar levels regularly or as instructed by their doctor. This can be done efficiently at home by using glucometers.
check their blood sugar levels regularly or as instructed by their doctor. This can be done efficiently at home by using glucometers.
