In the early 2000’s, a vaccine was released with a claim few vaccines could make; it could help prevent cancer. This seems like a bold claim, but what we know about Human Papilloma Virus (HPV) supports it. As of 2017, the vaccine has reduced cervical cancer cases by about 90% (New Study Points to Long-term Effectiveness of 9-Valent HPV Vaccine: Vaccine could prevent 90% of cervical cancer cases worldwide, 2017). However, since the release, it’s not been implemented as widely as doctors would have liked. Many of the objections parents have is that it’s a vaccine against a sexually transmitted virus, which is given to largely to young girls starting around age 11, well before they are expected to be sexually active.
What, exactly, is HPV, and why is it a big deal? Doctor Mike Evans gives a rundown of HPV on his YouTube channel DocMikeEvans, in a video titled “Should You Get the HPV Vaccine?”
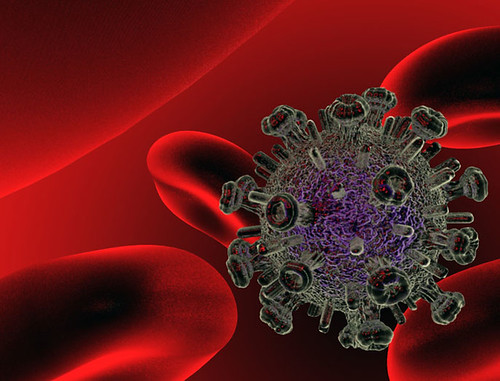
As Doctor Evans explains, warts caused by HPV can happen anywhere on the body. Of the many strains, or types of the virus, some are sexually transmitted and can cause warts on the genitalia. Two strains, known as strain 6 and strain 11, cause 90% of genital warts. I’m sure we can all agree that genital warts, though embarrassing and unpleasant, are not life-threatening. So, why is there a vaccine for it? Because some strains can cause cervical cancer, most commonly cervical cancer. HPV causes 99% of cervical cancers, with strains 16 and 18 causing a total of 70%. As Doctor Evans mentions, the virus can also cause cancer in the anus and penis as well. Many HPV infections are cleared by the body with no lasting effects, but a persistent infection can lead to cancer (Donken et al., 2020). Cervical cancer is one of the leading cause of death in women. Getting a diagnosis can be devastating. In this clip from WXXI News, discussing a documentary about the HPV vaccine, a woman’s story about her diagnosis is shown.
While the link between HPV and cervical cancer was made in 1999, the idea of viruses causing cancer has been around since the 50’s or 60’s. Doctor Sydney McElroy discusses the history of the HPV vaccine with her husband Justin in their podcast Sawbones: A Marital Tour of Misguided Medicine.
As Doctor McElroy notes, one of the biggest roadblocks in the way of getting adequate vaccination is the reaction parents have: “my kid doesn’t have sex.” But the point of a vaccine is to receive it before being exposed to the disease, so that the patient does not ever contract it.
The vaccine is usually given in three doses. Completing all the doses is necessary for the vaccine to be effective. It’s important to get parents on board when the time comes to give the vaccine. In 2020, only 47-52% of women age 19-24 had received all three doses, and a large contributing factor was how supportive of the vaccine their parents were (Rosen et al., 2020). Cervical cancer could be almost nonexistent if we can only make sure a vast majority of the at-risk population receives the HPV vaccine.
References
Donken, R., Hoes, J., Knol, M. J., Ogilvie, G. S., Dobson, S., King, A. J., Singer, J., Woestenberg, P. J., Bogaards, J. A., Meijer, C. J. L. M., & de Melker, H. E. (2020). Measuring vaccine effectiveness against persistent HPV infections: a comparison of different statistical approaches. BMC Infectious Diseases, 20(1), 1–11. https://doi.org/10.1186/s12879-020-05083-7
New Study Points to Long-term Effectiveness of 9-Valent HPV Vaccine: Vaccine could prevent 90% of cervical cancer cases worldwide. (2017). Contraceptive Technology Update, 1–3.
Rosen, B. L., Szucs, L. E., Wilson, K. L., Reyes, J. V., Fontenot, H. B., & Lee Smith, M. (2020). Factors associated with HPV vaccination before first sexual intercourse among female college students. Women’s Healthcare: A Clinical Journal for NPs, 8(1), 38–44.
