A controversial health concern I come across often in my practice as an RN is the decision whether or not to vaccinate newborns when they are first born. Many parents independently research the dangers of vaccinations and base their opinions and decisions off an article that they come across online, without determining the accuracy of the article. Often times, we form an opinion based off of what others are doing so whether it is a current trend to choose not to vaccinate or the opinion of a loved one, we are influenced by that. Despite many studies and years of parents vaccinating their babies with no issues, there are still parents that have strong feelings against vaccinating their children.
When a baby is born there are three standard vaccinations that are given to newborns, Hepatitis B, Vitamin K, and erythromycin eye ointment.
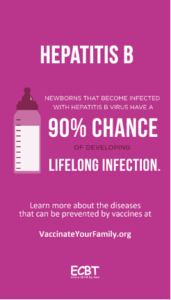
The reason the hepatitis B vaccine is standard for al babies is because mothers can unintentionally be a carrier of hepatitis B and pass it along to their newborns, the first dose is given within 24 hours of birth. Mothers chose not to give this vaccine, reason being because they know for a fact, they don’t have hepatitis B and they won’t let their baby be around anyone with hepatitis B or dirty needles. The issue with this is that they could have hepatitis B and not know it, or that someone that comes in contact with the newborn could have it and not be showing any symptoms.
Vitamin K is a necessary shot for newborns because most babies are
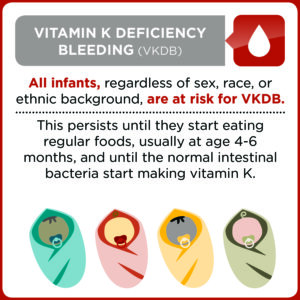 born without any vitamin K. Vitamin K is a clotting factor necessary to prevent hemorrhaging in newborns. The reasoning behind parents refusing this for their children, is that they fear their child could be potentially allergic, they think it is unnecessary in uncomplicated births, they also fear that this could be toxic to their newborn. Although complications from the vitamin K shot are extremely rare, and the benefits outweigh the risks parents still chose to decline the shot, the shot has been standard for newborns since 1961.
born without any vitamin K. Vitamin K is a clotting factor necessary to prevent hemorrhaging in newborns. The reasoning behind parents refusing this for their children, is that they fear their child could be potentially allergic, they think it is unnecessary in uncomplicated births, they also fear that this could be toxic to their newborn. Although complications from the vitamin K shot are extremely rare, and the benefits outweigh the risks parents still chose to decline the shot, the shot has been standard for newborns since 1961.

Erythromycin eye ointment has been used for newborns since the 1800’s. This practice started as a way to prevent ophthalmia neonatorum, and illness that can cause blindness in newborns. Often times parents reasoning for declining the eye ointment is because they fear their newborn will b
e irritated from it or develop chemical conjunctivitis another reason parents sometimes decline is because they know they do not have an STI. The reason this eye ointment is given is to protect the baby’s eyes from STI’s but other common bacteria as well.
When it comes to vaccinations, do what you think is right, but make sure yo
u are making an informed decision with you child’s best interest in mind.
Sources:
Centers for Disease Control and Prevention. (2020, February 25). Baby vaccines at birth. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/parents/by
-age/newborn-birth.html#:~:text=Hepatitis%20B%20(HepB)&text=Mothers%20can%20unknowingly%20pass%20the,within%2024%20hours%20of%20birth.&text=If%20you%20have%20hepatitis%20B,within%2012%20hours%20of%20birth.
Centers for Disease Control and Prevention. (2021, January 1). Protect babies from life-threatening bleeding – talk to expectant parents about the benefits of the vitamin K shot for newborns. Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/vitamink/vitamin-k-fact-sheet-
hcp.html#:~:text=Although%20the%20Vitamin%20K%20shot,and%20misperceptions%20about%20its%20safety.
Dekker, R. (2021, October 25). Evidence on erythromycin eye ointment for newborns. Evidence Based Birth®. https://evidencebasedbirth.com/is-erythromycin-eye-ointment-always-necessary-for-newborns/
Hallas, Donna; 1Altman, Susan; 2Mandel, Elizabeth; 3Fletcher, Jason4. (2023, March 27). Vaccine hesitancy in prenatal women and mothers of newborns: Results of an interventional study. EBSCO host. https://web-s-ebscohost-com.ezproxy.neit.edu/ehost/detail/detail?vid=3
&sid=7419518a-7253-4069-bc7d-842c5fb687e4%40redis&bdata=JnNpdGU9ZWhvc3QtbGl2ZQ%3d%3d#AN=162025119&db=ccm
Loyal, J., Weiss, T. R., Cheng, J. H., Kair, L. R., & Colson, E. (2019). Refusal of vitamin K by parents of newborns: A qualitative study. Academic pediatrics. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7028442/#:~:text=Why%20parents%20refuse%20IM%20vitamin,belief%20that%20it%20is%20unnecessary.
Ramirez, C. A., Garner, C. D., & Whale, T. H. (2021, January 1). Neonatal vitamin K refusal increasing. InfantRisk Center. https://www.infantrisk.com/content/neonatal-vitamin-k-refusal-increasing#:~:text=During%20cases%20of%20late%2Donset,they%20have%20a%20brain%20bleed.&text=One%20study%20found%20that%20the,uncomplicated%20births%20of%20healthy%20infants.