
Occupational therapy and traumatic brain injury
Occupational therapy is critical in the recovery from a traumatic brain injury (TBI) in which it helps with teaching patient’s how to regain their functional independence. This is essential for adjusting to life after a TBI and facilitating a safe and successful recovery back to participating in daily activities. As an occupational therapy practitioner working with a traumatic brain injury patient, it is important to know different treatment options and the evidence that supports the interventions chosen for a specific patient. This blog goes into different scholarly articles and media sites that discuss occupational therapy and brain injury. The question is, which source would be better to base clinical intervention’s on when treating a patient with traumatic brain injury?
Below is what the media says about occupational therapy and traumatic brain injury:
The above video “Occupational Therapy and Neuroplasticity After Brain Injury” is a video by Dr. Shawn Phipps who has been an occupational therapist for 21 years. Dr. Phillips discusses a case on a patient named Armando Rodriguez who had a severe TBI from falling asleep behind the wheel of a car and got into an accident. He was in a coma for about a week. Once Armando was stable, he was very agitated in which he didn’t know who he was, where he was or what happened. He was then transferred to Ranchos Los Amigos Rehabilitation Center.
Every part of Armandos brain was affected from the TBI including his: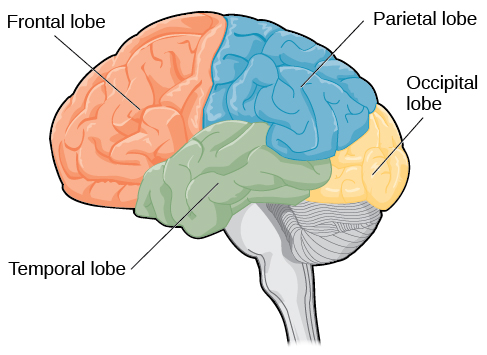
- Frontal lobe: which involves reasoning, planning, speech, movement, problem solving and emotions.
- Parietal lobe: which involves sensory integration, touch pressure, spatial orientation, temperature, information processing.
- Occipital lobe: which involves visual processing.
- Temporal lobe: which involves auditory stimuli, memory and speech.
The brain controls everything from how we preform daily activities, how we move, how we communicate, sense, feel, think and make decisions.
Dr. Philipps discussed how neuroplasticity is the ability for the brain to change in response to challenge, action, practice and evaluation. When Dr. Philips began working with Armando, he was unable to focus on a specific task for more than a few seconds before his brain fought sensory overload. Over time, Armando’s attention would get better by fighting the urge to loose focus. When treating traumatic brain injury clients, it is important to challenge patients and practice activities daily in which it creates new pathways in the brain.
After working with Armando daily, Dr. Philips created a specific routine and structure for Armando to participate in to aid in the neuroplasticity in his brain, as well as connect the pathways that have been affected by this injury. By doing so, Armando eventually became independent and was able to return to his normal life which included being a manager at the restaurant like he was prior to the TBI. (Phillips, S 2019).
In the above video “What OT can do for you: Traumatic Brain Injury (TBI)” it has an Occupational Therapist named Kelsey Watters discuss how working with traumatic brain injury is difficult but rewarding. In the video, Kelsey is working with a patient named Scott who had a TBI. By using activities that he was interested in prior to the accident helps motivate Scott with participating in treatment sessions. For example, since Scott was a race-car driver, she gave Scott a driving wheel to hold and use to help with object recognition and encourage movement in his upper extremities. Kelsey’s treatment sessions with Scott are very client centered and engaging to promote his participation in familiar tasks. Other therapists didn’t think Scott would make it as far as he has however, with Kelsey as his occupational therapist he continues to improve every day through the use of activities he enjoys. (The American Occupational Therapy Association, 2017).
In the video “The Road to Recovery Following Brain Injury” it discusses how brain injury truly affects a person’s life functions such as thinking, social emotional, and physical aspects of daily life. Symptoms can range from mild to severe in which affects each patient’s treatment differently. Although it is impossible to really predict the treatment and outcomes from TBI, it is important to start treatment early for a better recovery.
When a person goes through a traumatic event involving a brain injury, typically the patient will be admitted to the emergency room. If the patient’s situation is severe, they will be transferred to an intensive care unit (ICU) where they will help aid the patient in becoming medically stable. Once the patient is stable and aware, they will be transferred to an acute care floor where the patient receives intense rehabilitation. If they can continue to benefit from rehabilitation weeks later the patient will be transferred to an inpatient rehabilitation center, if not they will be sent home and go to outpatient services which focuses on community reintegration.
The above video also goes into discussing that by understanding how brain tissue and neuroplasticity works, it creates more of a desire for rehabilitation to help rewire the brain. By doing so, this helps with the progression of a patient’s recovery to improve their participation and performance in functional activities. Structure and a solid support system are vital in the recovery process for individuals with TBI. The overall goal is to help the patient towards being as independent as possible and to return to their daily lives and routine. It is a difficult road to recovery but totally possible with individuals who face traumatic brain injury. (AHSchannel, 2014).
Each of the above media sources share similar information however the information is very focused on the specific patient that the specific media clip is talking about. There is some scientific-evidence in these sources however, the sources don’t go in depth about traumatic brain injury as a whole. These videos are each consistent with the facts about traumatic brain injury in which allows the audience to trust these sources of information.
Below are scholarly articles and what they say about occupational therapy and traumatic brain injury:

A patient working on their fine motor skills during a treatment session with an occupational therapist, By: Marco Bloomfield.
The article “Effectiveness of Interventions Within the Scope of Occupational Therapy Practice to Improve Motor Function of People With Traumatic Brain Injury: A Systematic Review”, discusses the evidence of the motor interventions of occupational therapy for individuals with TBI. The ages of the participants in this study ranged from 12-76 years old and the ranges of the brain injuries varied from mild to severe. Since the ranges of the brain injuries varied, the rehabilitation programs varied as well. The more severe the brain injury, the more intense the rehab. Throughout the rehabilitation process, the occupational therapist worked with each person differently in which they had different goals. It was evident that the patients who had a less severe TBI, motor function progressed faster than those with a more severe TBI.
“Moderate evidence in this study indicates that various exercise programs provide benefits for motor function, including decreased spasticity, increased isolated hand movement, increased physical activities, improved strength and functional reach, and improved balance” (Pei-Fen, 2016). There is limited data from the study suggests that rehabilitation and computer-based programs can help patients with TBI improve their motor function. Since motor function is critical to most performance abilities and rehabilitation is hindered by other impairments, such as cognitive and sensory function, occupational therapy interventions that encompass the essential areas of motor function must be developed and implemented by an occupational therapist. Motor function encompasses a wide range of abilities, and additional impairments, such as cognitive and sensory function, make recovery more difficult. The requirement for occupation-based standardized outcome measurements and interventions for motor function recovery after TBI have been proved in this study that it is most beneficial to be met by occupational therapists. (Pei-Fen J, 2016).
Living with a traumatic brain injury can mean a long road to recovery.

Kevin in the outpatient day program participating in a cooking program with his therapist, Nikki, By: Gerry Gianacola.
The article “Occupational Therapy Interventions for Adults With Traumatic Brain Injury” goes into a case on a 33 year old man, Kevin, who had a TBI from falling 28 feet into concrete. Kevin was then brought to the hospital and was transferred onto the intensive care unit (ICU) where he was vented. He was on this unit for about a month where he was then transferred to an inpatient rehabilitation hospital for 3 months. After he completed the rehabilitation program at this hospital, he was transferred home with his wife where he got more rehabilitation from an outpatient brain injury day program.
Nikki was Kevins occupational therapist at the outpatient brain injury day program. Nikki created goals for Kevin to accomplish while he was in the program that were client centered and focused on his community integration skills, motor skills, memory and self awareness. Kevin also expressed how he was feeling depressed in which limits him from doing his best in therapy sessions. He had difficulties comprehending and managing with the emotions of life after the TBI, as well as an inability to participate in activities he loved prior to the incident. Kevin began engaging in a physical exercise program at the outpatient day treatment facility’s aquatic therapy pool. Kevin exercised for a minimum of 90 minutes each week to reduce stress, sadness, anger, fatigue, and enhance his overall well being.
After 6 months of rigorous therapy sessions, Kevin met his goals and had improved overall. Despite his progress in occupational therapy, Kevin is not exactly where he would like to be and is faced with a difficult and uncertain future. The road to a more productive daily routine may be rocky, as new tasks put current cognitive, physical, psychological, and emotional skills to the test, as well as raising expectations of increased independency. Kevin’s next step is career exploration and return to work; depending upon the needs of his employment, his symptoms, and his current supports, Kevin may require more engagement in different areas of the rehabilitation system. (Wheeler, S. 2017).
Occupational therapists focus the patient as a whole, which can include focusing on visual deficits.

A patient visual tracking objects with an occupational therapist, By: Andrea Sanchez.
The article “Effectiveness of Interventions to Address Visual and Visual-Perceptual Impairments to Improve Occupational Performance in Adults with Traumatic Brain Injury” discusses how with traumatic brain injury (TBI), visual and visual–perceptual deficits are common and have an impact on occupational performance. The effectiveness of therapies within the framework of occupational therapy to enhance daily functioning for persons with visual and visual–perceptual deficits as a result of TBI was investigated in this comprehensive study. “This systematic review is one of six reviews of the TBI literature relevant to occupational therapy conducted under the auspices of the American Occupational Therapy Association (AOTA) Evidence-Based Practice (EBP) Project” (Berger, 2016).
The evidence on occupational therapy for people with visual and visual–perceptual impairments caused by a TBI within the realm of occupational therapy practice is broad. The research examined shows that scanning can be used as a compensatory method to enhance computer visual search abilities in persons with visual field deficiencies. Audiovisual stimulation is supported by moderate research for patients with visual field impairments or oculomotor issues. The article discusses how TBI patients have a variety of issues in addition to vision loss, such as cognitive and physical limitations. These unique restrictions may have an impact on the efficacy of therapies designed for different groups. Occupational therapy practitioners treating patients who had a TBI must recognize the consequences of visual and visual–perceptual impairments for occupational success and select therapies based on their rationale and data available based on the patient’s overall injury. (Berger, S, 2016).

 Is the media really trustworthy when choosing interventions for traumatic brain injury patients, compared to evidence based articles?
Is the media really trustworthy when choosing interventions for traumatic brain injury patients, compared to evidence based articles?
The information provided by the above media clips did align with a lot of the information provided in the evidence-based sources. The media goes into how traumatic brain injuries can range from mild to severe and may require different roads in the rehabilitation process. The media also goes into how neuroplasticity, structure and challenge play a huge role in the recovery process. Although this is all very important information, the media tends to focus more on a specific type of client and what their story is, rather than traumatic brain injury as a whole. The media also tends to lack evidence and doesn’t provide the person watching with any clinical reasoning. The information tends to go more in-depth with scholarly sources on interventions and the focus on traumatic brain injury as a whole diagnosis.
In conclusion: The evidence above has shown how occupational therapy is beneficial for individuals with traumatic brain injury however, the significance of occupational therapy treatment in traumatic brain injury rehabilitation was not clearly stated in the media segments. Anyone could upload info on the internet, and there are no restrictions on who can do so. If an expert decides to share a scholarly article, there are rules to follow to guarantee that the material is correct and that acknowledgement is given to other sources. Although there was some common information between the media and evidence-based articles, I would not fully trust what you see on the media compared to what you read in a scholarly article when choosing an intervention for a patient. The overall professional understanding and knowledge from the experts writing the article is what makes the source reliable. If you do prefer to watch videos and media, it is recommended to fact check the information you find via scholarly and peer reviewed articles for confirmation on occupational therapy interventions for patients with traumatic brain injury.
Written by: Kaitlyn Carvelli
References:
AHSchannel (2014), “The Road to Recovery Following Brain Injury” https://www.youtube.com/watch?v=3pCiWDKA93s
Berger, S., (2016). Effectiveness of Interventions to Address Visual and Visual-Perceptual Impairments to Improve Occupational Performance in Adults with Traumatic Brain Injury: A Systematic Review. American Journal of Occupational Therapy, 70(3), p1–p7. https://doi.org/10.5014/ajot.2016.020875
Pei-Fen J. (2016). Effectiveness of Interventions Within the Scope of Occupational Therapy Practice to Improve Motor Function of People With Traumatic Brain Injury: A Systematic Review. American Journal of Occupational Therapy, 70(3), p1–p5. https://doi.org/10.5014/ajot.2016.020867
Phillips, S (2019), “Occupational Therapy and Neuroplasticity After Brain Injury”. https://www.youtube.com/watch?v=AEzsxKQ3Gfc
Radomski, M. (2009). Occupational Therapy for Service Members With Mild Traumatic Brain Injury. American Journal of Occupational Therapy, 63(5), 646–655. https://doi.org/10.5014/ajot.63.5.646
The American Occupational Therapy Association, (2017). “What OT can do for you: Traumatic Brain Injury”. https://www.youtube.com/watch?v=a_SROgPA2GM
Wheeler, S., (2017). Occupational Therapy Interventions for Adults With Traumatic Brain Injury. American Journal of Occupational Therapy, 71(3), 1–3. https://doi.org/10.5014/ajot.2017.713005
