What is Frozen Shoulder?
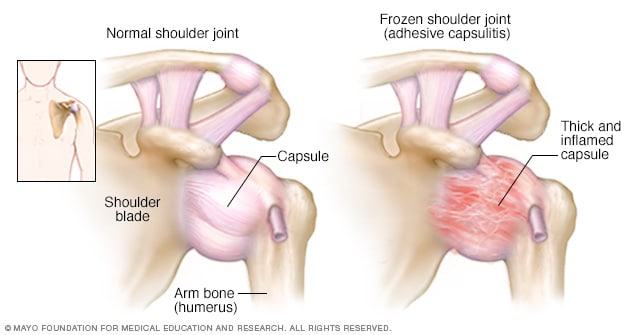
Frozen shoulder is one of the most common conditions characterized by severe pain in the shoulder area and deficits in movement. It primarily affects individuals in their forties to sixties and is more common in women. According to the Mayo Clinic website, certain health conditions, such as diabetes, thyroid issues, heart conditions, Parkinson’s disease, stroke, and prolonged immobility of the shoulder can cause Frozen Shoulder symptoms.
Frozen Shoulder Onset and Phases of Pain and Stiffness
According to research, the onset of frozen shoulder can be sudden and subtle and gets worse over time. Loss of joint mobility, both active and passive is a telltale sign of a Frozen shoulder, however, it can often be wrongly diagnosed as other shoulder conditions such as osteoarthritis or a tear in the rotator cuff.
According to experts, it occurs in three stages:
- Freezing Stage: the most pain, some stiffness.
- Frozen Stage: subsiding pain, loss of movement
- Thawing Stage: the gradual return of movement in the joint, passive as well as active.
Each of these stages may last from several months to years. (Chan, et al., 2017), (Georgiannos, et al., 2017)
Best Approaches to Treatment
Although several articles discuss and describe the best treatment approaches for adhesive capsulitis, the article by Georgiannos, D., Markopoulos, G., Devetzi, E., & Bisbinas, I. (2017). offers a comprehensive review of the available and most reliable treatment options in each stage of the condition.
The authors describe adhesive capsulitis of the shoulder (ACS) as a motion limiting condition which is mainly characterized by pain and the restriction of active and passive movements in the shoulder and arm. According to the article, the pathophysiology of ACS is poorly understood, as it is clinically characterized by the different stages of pain and stiffness.
The educational video below, by Nabil Ebraheim, M.D. from the University of Toledo medical center describes with great accuracy and detail the etiology, course of development, and signs and symptoms of frozen shoulder. However, it provides less detail about the available treatment options and the best approaches to treatment in each stage of the condition.
Overall, the media clip below presents a credible and reliable source to understand and educate oneself on ACS.
Physical Therapy and Exercise for Adhesive Capsulitis (Frozen Shoulder)
Physical therapy and home exercises are used as the first-line of treatment with patients with ACS. All the articles and the media clips reviewed for this blog report that physical therapy and exercise, together with anti-inflammatory medications such as Advil, Motrin, Naproxen, Celebrex are an initial course of treatment for this condition. However, diagnostic tests, such as Xray, MRIs, and a visit to the doctor to rule out any other shoulder conditions are important.
In addition, the article by Redler, L.H.,& Dennis, E.R. (2019) “Treatment of adhesive capsulitis of the shoulder” notes that when early corticosteroid injections are administered there has been a decrease in the amount of time that the symptoms last. The research identifies how physical therapy has been shown to minimize pain relief and promote the return of functional movement in the shoulder. Additionally, when used in combination with physical therapy, intra-articular corticosteroids resulted in better outcomes compared to the use of only intra-articular corticosteroids. (Chan, et al., 2017)
The media clip below is the presentation from the physical therapist Marike Louw from the online physio clinic “Sports Injury Physio”, where she underlines the importance of getting corticosteroid injections in the early, painful stage of the conditions in conjunction with therapy and the home exercise program.
Is Surgery the Answer?
In some instances, when the pain and movement do not resolve with all other available treatments, doctors may recommend surgery. However, the research reports that there is no conclusive evidence to show that early operative treatments, such as manipulation under anesthesia (MUA) and surgical capsular release are a more effective course of action. (Yip, et al., 2018)
Physical therapist Marike Louw, in the video clip above, mentions that with physical therapy, corticosteroid as well as hydrodistention injection, there is no need to refer the patient for surgery. However, according to orthopedic surgeon Dr Bennet (below), if the shoulder movement reaches the frozen stage, a surgical capsular release is necessary.
In conclusion
Frozen shoulder can be debilitating to people for prolonged periods of time, which is why understanding the best approaches for treatment and seeking professional help is very important. As the research and media review indicates, starting the treatment early on could affect the severity and the length of the condition and could be the deciding factor whether or not the surgery may be needed.
Overall, the information presented in the media clips accurately reflects the information presented in scholarly articles, however, seeking professional help, relying on diagnostic tests, and following the recommendations of your healthcare provider is of utmost importance.
References
Chan, H. B. Y., Pua, P. Y., & How, C. H. (2017). Physical therapy in the management of frozen shoulder. Singapore medical journal, 58(12), 685.
Georgiannos, D., Markopoulos, G., Devetzi, E., & Bisbinas, I. (2017). Adhesive capsulitis of the shoulder. Is there consensus regarding the treatment? A comprehensive review. The open orthopedics journal, 11, 65.
Redler, L.H.,& Dennis, E.R. (2019). Treatment of adhesive capsulitis of the shoulder. JAAOS-Journal of the American Academy of Orthopaedic Surgeons, (27), e544-e544.
Yip, M., Francis, A. M., Roberts, T., Rokito, A., Zuckerman, J. D., & Virk, M. S. (2018). Treatment of adhesive capsulitis of the shoulder: A critical analysis review. JBJS reviews, 6(6), e5.
Mayo Clinic. (n.d.). Frozen Shoulder. Retrieved November 17, 2021 from https://www.mayoclinic.org/diseases-conditions/frozen-shoulder/symptoms-causes/syc-20372684
Ebraheim,N. (2011). Adhesive capsulitis, frozen shoulder: Everything you need to know. [Video]. YouTube. https://www.youtube.com/watch?v=mgXknwC2X7g
Bennet, M. J. (2014). Frozen shoulder adhesive capsulitis. [Video]. YouTube. https://www.youtube.com/watch?v=h1vj9JaxCqQ&t=38s
Sports Injury Physio. (2019). Frozen Shoulder- Causes and treatment. [Video]. YouTube. https://www.youtube.com/watch?v=iKlQMHrJiUQ